
Table of Contents ▾
The bulbospongiosus is a small but powerful muscle at the base of the genitals, wrapping around the perineal body. Because it’s involved in pumping blood into the clitoris or penis, any tension or dysfunction in this muscle shows up quickly and unmistakably.
Pain in the bulbospongiosus often feels like a dull ache in the perineum. You can also experience a burning sensation at the genital base, or a sharp, tight pressure that intensifies during arousal or after orgasm.
When it loses the ability to relax, the entire sexual response cycle becomes strained, and the body can’t complete the natural rhythm that makes orgasm satisfying instead of painful.
In this article, we’re going to break down what the bulbospongiosus is, why pain develops, and how to heal it through both physical release techniques and somatic, nervous-system-based practices that support long-term relief.
Anatomy of the Bulbospongiosus and Pelvic Floor
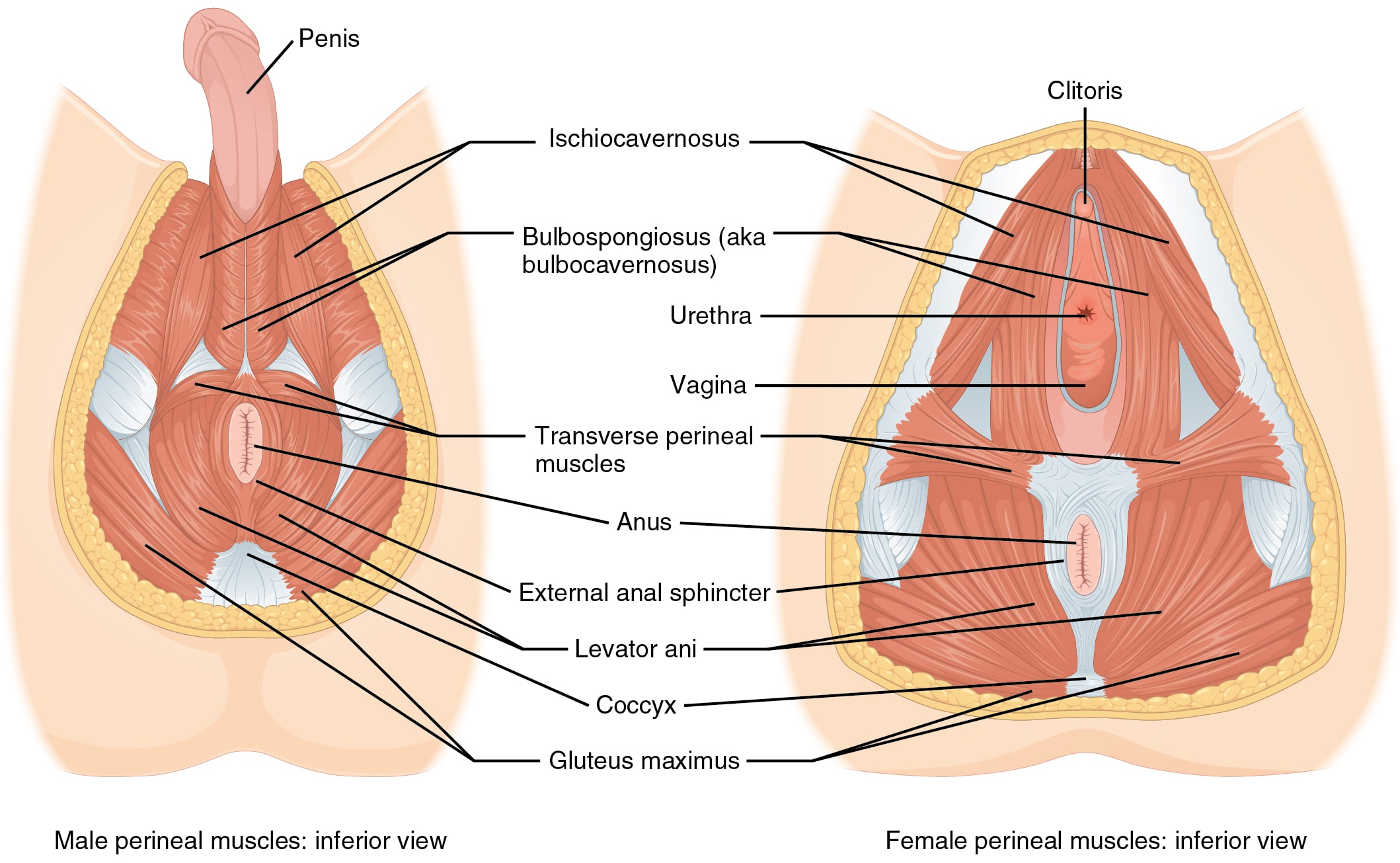
The bulbospongiosus is part of the superficial layer of the pelvic floor, lying just beneath the perineal skin and wrapping around the root of the genitals like a small but powerful muscular bowl. Anatomically, it anchors into the central tendon of the perineum which is the meeting point for multiple pelvic structures.
Because of this placement, the bulbospongiosus contracts and relaxes in a coordinated rhythm with the ischiocavernosus, the superficial transverse perineal muscle, the external sphincters, and the deeper levator ani group. These muscles together form the urogenital triangle, maintaining pelvic integrity during everyday movement.
In men, the bulbospongiosus wraps firmly around the bulb of the penis and the proximal portion of the penile urethra. When it contracts, it creates a pumping action that helps propel semen during ejaculation and expel the last drops of urine.
In women, the same muscle takes on a slightly different but equally essential role. Rather than pumping along a urethral tube, it wraps around the vestibule of the vagina and the roots of the clitoral network, the bulbs of the vestibule. When it contracts during arousal, it narrows the vaginal entrance slightly, enhances the swelling of the clitoral bulbs, and works together with the ischiocavernosus to maintain clitoral engorgement.
The Pundendal Nerve
Threaded through this entire region is the pudendal nerve, the primary sensory and motor nerve of the pelvic floor. It travels through a narrow anatomical passageway, branches into the perineum, and supplies sensation to the clitoris or penis, the labia or scrotum, the perineum, and the anal region.
Because the nerve runs directly beneath and between the superficial pelvic muscles, tension in the bulbospongiosus can easily compress or irritate it. When this happens, the pain rarely stays confined to the exact spot of the muscle. Instead, the discomfort spreads outward along the nerve’s distribution pattern, sometimes presenting as burning at the clitoral hood, aching in the scrotum, hypersensitivity along the vulva, or a deep, electric pressure in the anus. Many people describe it as if the entire pelvis is being “pulled inward,” “electrified,” or “shut down,” when in reality much of the irritation traces back to this single, overactive muscle.
Causes of Bulbospongiosus Pain
1. Chronic Overactive Gripping
The most common cause of bulbospongiosus pain is subtle, habitual clenching of the pelvic floor. Many people unconsciously grip their perineum and over time, this low-grade tension becomes a default pattern. The bulbospongiosus never fully relaxes and the muscle becomes tender and easily irritated.
2. Pudendal Nerve Compression from Posture or Activities
Prolonged sitting can compress the pudendal nerve where it runs beneath the perineum. Activities like cycling, rowing, and horseback riding increase pressure in this region and can irritate the nerve until it begins firing pain signals with even small movements. Because the bulbospongiosus lies directly over the nerve’s pathway, any muscle tightness amplifies the irritation, creating radiating pain into the genitals, anus, or groin.
3. Sexual Tension, Strain, and Incomplete Arousal
The bulbospongiosus is highly active during arousal and orgasm. When ejaculation is forced, penetration begins before the body is fully ready, or an orgasm is chased with excessive muscular effort, the tissue can contract too hard and fail to release afterward. Instead of relaxation, the muscle stays partially locked, creating burning, soreness, or sharp pain during the next arousal cycle. Over time, this can create a loop where sexual attempts automatically trigger guarding or tension.
4. Scar Tissue from Childbirth, Surgeries, or Past Injuries
The perineum is a central meeting point for multiple pelvic-floor structures. Any injury here can lead to scar tissue or adhesions. These adhesions reduce elasticity and alter the way the bulbospongiosus contracts. When the surrounding tissue loses its glide, the muscle has to work harder to achieve the same movement and often becomes fatigued and painful.
5. Somatic and Emotional Holding Patterns
The pelvic floor is deeply influenced by the nervous system. Stress and negative emotions can keep the bulbospongiosus in a guarded state long after the original trigger is gone. The body learns to protect itself through clenching, and this pattern becomes wired into the musculature. Even when someone consciously feels fine, the pelvic floor may still be holding onto old bracing patterns that manifest as burning, pressure, or hypersensitivity.
6. High-Intensity Workouts or Mismanaged Core Training
Heavy lifting, high-intensity interval training, or aggressive core exercises can create downward pressure into the pelvic floor. Without proper coordination, the bulbospongiosus may overcompensate to stabilize the pelvis. This often leads to delayed soreness or pain during sexual activity, especially in people who habitually “brace the core” without pelvic-floor awareness.
7. Hormonal Shifts Affecting Tissue Irritability
Changes in estrogen levels can make the vulvar and perineal tissues more sensitive and less hydrated. While the bulbospongiosus is a muscle, it interacts with surrounding fascia and glands that depend on estrogen for comfort and elasticity. When these tissues are irritated, the muscle often tightens defensively, creating a cycle of pain and contraction.
Practices for Healthy Pelvic Floor Muscles
1. External Perineal Pressure
External perineal pressure is one of the most direct ways to work with the bulbospongiosus because it meets the muscle exactly where it contracts at the surface. This practice involves applying slow, steady contact to the perineal body using warm hands or the broad base of a smooth crystal wand or pelvic massager. The steady pressure gives the nervous system a predictable, non-threatening sensation. Over time, this helps override the instinctive guarding response that keeps the bulbospongiosus tight.
As the pressure settles in, the body begins to identify where it is holding and where it can soften. Because the bulbospongiosus is part of the superficial pelvic floor, this technique works well for the type of tightness that shows up as surface-level burning or aching. When practiced with slow breathing and plenty of time, the tissue gradually becomes more pliable, and the reflexive clench around the perineum starts to dissolve.
2. Wand Work

Working internally with a wand made of glass, stainless steel, or a crystal wand offers pressure and engagement that fingers can’t always provide. The vaginal entrance is one of the primary places the bulbospongiosus contracts, almost like a muscular ring that tightens when the body anticipates something. Using a wand here allows for slow exploration, helping the body re-learn how to differentiate between gentle pressure and threat.
The key to this practice is working just inside the entrance, not deep inside the vaginal canal. A few centimeters are enough to connect with the rim of tissue where most people carry unconscious gripping. With slow, small movements the tissue begins to soften. What makes this effective is the muscle can feel the difference between gripping and releasing. Over repeated sessions, the nervous system becomes less reactive and the area gains a more responsive elasticity.
3. Crystal Anal Plugs

While the bulbospongiosus sits toward the front of the perineum, the entire pelvic floor functions as a coordinated system. Tension at the back of the pelvic floor often directly influences tension at the front. A crystal anal plug, used gently and with plenty of lubrication, provides constant sensory feedback that makes unconscious gripping impossible to ignore. The slightest contraction immediately changes the sensation and the slightest release brings noticeable softening.
This practice helps identify the difference between resting tone and protective bracing, something many people have never consciously felt. Once inserted, as the pelvic floor softens on the inhale, the plug shifts slightly; as the exhale melts the tissues, the pressure decreases. Over time, the body learns what true relaxation feels like in an area where many people unknowingly hold tension all day. This is particularly helpful for people who clench without realizing it or experience pain that feels diffuse or hard to pinpoint.
4. Somatic Breathing
Deep pelvic release comes from restoring natural movement patterns. The diaphragm and pelvic floor mirror each other. When you inhale, the diaphragm moves downward, and the pelvic floor is meant to soften and expand with it. When you exhale, both gently recoil. But in states of chronic stress or bracing, this rhythm becomes disrupted. Many people unknowingly inhale while tightening the pelvic floor, or hold their breath during any sensation they find uncomfortable.
By directing the breath into the lower belly and pelvic bowl, the nervous system receives a signal that it is safe to loosen its grip. This rhythm lowers overall pelvic tone and reduces the reactive, protective tightening that underlies so much bulbospongiosus pain.
Read: Pelvic Floor and Breathing Coordination
5. Sound, Vagal Activation, and Nervous-System Downregulation
Sound is an underrated but powerful part of pelvic release. Letting sound move through the throat during exhalation activates the vagus nerve, shifting the body away from fight-or-flight and into a state where the pelvic floor can relax voluntarily. Sound prevents the breath from freezing and guides the nervous system into openness. When sound is paired with external or internal work the pelvic floor receives clear cues that it is safe to soften.
6. Micro-Movements and Pelvic Mobility
Hip position, sacral mobility, and even how you hold your lower back all influence how the bulbospongiosus behaves. Small, deliberate movements through trying simple practices like pelvic rocks, hip circles, and figure-eights change the length of the pelvic floor subtly and continuously.
These movements also help integrate the release work into daily life. Many people can relax the pelvic floor during a session but immediately return to clenching as soon as they go about their daily lives. Mobility practices retrain the body to remain relaxed during motion, which is ultimately what resolves pain long-term. The more the pelvis can move freely, the less the bulbospongiosus has to overwork as a stabilizer.
7. Pelvic Floor Physical Therapy
Pelvic floor physical therapists are the frontline specialists for bulbospongiosus pain because they can assess the muscle directly and feel the patterns you can’t access on your own. A trained clinician can identify whether the muscle is overactive, underactive, full of trigger points, or being pulled tight by surrounding structures.
They may use gentle internal pressure, myofascial techniques, and targeted mobilization to release the muscle safely. But the real value is in learning how to relax during inhalation and how to let the muscle lengthen instead of gripping automatically. Many therapists also use EMG or sensor-based biofeedback to help you see when you’re clenching and when you’re actually letting go.
8. Lifestyle Adjustments
Before reaching for complex techniques, it’s worth looking at the daily habits that quietly keep the bulbospongiosus irritated. Small changes can make a noticeable difference.
Below are simple adjustments that create a healthier baseline for the rest of your pelvic floor work:
-
Switch to softer seating and reduce perineal pressure
-
Break up long sitting periods
-
Adjust your posture, especially the tailbone tuck
-
Stay hydrated to support easy elimination
-
Reduce straining on the toilet
-
Pace sexual activity rather than rushing arousal
-
Give yourself recovery time after sex
-
Wear clothing that doesn’t compress the perineum
A Clear, Supportive Path Forward: The Healing Vaginal Pain Course
If you’re looking for a structured way to understand your vaginal or perineal pain and actually learn how to shift it, the Healing Vaginal Pain course by The Empowered Woman gives you a grounded, step-by-step path.
Natasha, who healed her own pelvic pain, and Courtney Davis, founder of The Empowered Woman, teach you the exact physical and somatic tools that help the pelvic floor soften and rebuild trust.
This course is ideal for women who feel tension or guarding in the vaginal entrance or perineal area and want guidance they can follow at home. It’s especially supportive if you’ve tried scattered advice with no real change and are ready for a clear method.
Inside the program, you’ll find 11 modules and 58 short lessons that break everything down into manageable practices. You’ll learn simple assessments so you can understand exactly what your own pattern is. From there, the course teaches hands-on techniques and you’ll also learn somatic tools like breathwork and nervous-system pacing to help your body let go of its protective patterns.
Conclusion
Bulbospongiosus pain doesn’t arise from one simple cause. It’s often a mix of physical tension, old holding patterns in the pelvic floor, and emotional or nervous-system responses that have been shaping the way the body protects itself. When this muscle hurts, it’s usually because something deeper has been asking for attention for a long time.
The good news is that there are many ways to support your own healing. When you slow down and actually tune in to the area the pain often begins to soften. Awareness itself is a powerful intervention. It helps you understand what the muscle is doing and what it needs in order to let go.
With time, a combination of gentle self-release, mindful breath, nervous-system calming, and small daily adjustments can make a significant difference. The bulbospongiosus responds well to consistency and presence. As you create more safety in the body, the tension that once felt fixed or overwhelming can begin to unwind.
FAQ
The bulbospongiosus muscle often becomes painful when it’s carrying more tension than the body can regulate. This muscle is part of the superficial pelvic floor muscles, and it contracts during urination, orgasm, ejaculation, and stress. When someone develops pelvic floor overactivity, the BS can stay partially engaged all day, especially during prolonged sitting, workouts, sexual arousal, or even mild anxiety. This constant low-level contraction limits blood flow, irritates nearby branches of the pudendal nerve and perineal nerve, and creates trigger points that refer pain into the penis, clitoris, vagina, anus, and lower abdomen.
In men this may also affect penile erection, penile rigidity, or contribute to ejaculatory pain, because the BS helps press on the deep dorsal veins and influences erectile function. Scar tissue from childbirth, surgery, or past injuries can also make the connective tissue less mobile, forcing the bulbospongiosus to work harder. A skilled pelvic floor physical therapist can evaluate these patterns with manual therapy, surface EMG, and a targeted physical exam to determine whether the pain stems from muscle tension, pudendal nerve irritation, or a combination of both.
Pain at the top of the pubic bone is often muscular rather than bony. The pelvic floor, abdominal wall, and soft tissue of the pelvic region all anchor into the anterior pelvis, so when the levator ani muscles, the ischiocavernosus muscles, or the bulbospongiosus tighten, they can pull on the attachments along the pubic symphysis. This creates a sharp or aching sensation that many people mistake for a joint problem.
In reality, it’s usually part of a larger pattern of pelvic floor dysfunction, where tension, posture, or chronic pelvic guarding irritate the afferent fibers and nerve pathways that run along the front of the pelvis. Because the pudendal nerve and dorsal nerve of the clitoris or penis run close to this region, irritation can easily refer pain to the pubic bone, groin, and lower abdomen. Many patients with chronic pelvic pain syndromes describe this discomfort as shifting from the pubic bone to the perineum or even into the testicles.
A sore pelvic floor rarely feels like one isolated point of pain. Most people describe a blend of deep aching, burning, pulling, or pressure across the perineum, anus, and genitals. Because the pelvic floor contains interconnected muscles likethe external anal sphincter, the external urethral sphincter, and the levator ani, any irritation can spread quickly through shared nerves and fascia. People with pelvic floor soreness often feel a sense of heaviness in the pelvic region, pain that intensifies during sitting or sexual intercourse, or sensations that shoot into the penis, vulva, vagina, testicles, or pubic bone.
This is classic referred pain, where muscle tension or pudendal neuralgia sends mixed messages along the nerve pathways. For many, a sore pelvic floor also comes with difficulty relaxing after bowel movements or sexual activity, since the nervous system keeps the perineal muscles ready to contract. This “on edge” feeling is common in chronic pelvic pain, especially when the pelvic diaphragm and surrounding soft tissue are irritated from long-term guarding.
Relaxing the bulbospongiosus muscles requires addressing both the tissue and the nervous system. Because the BS is involved in sexual response, ejaculation, bodily protection, and urethral control, it can’t simply be “stretched.” What helps most is a combination of somatic breathing, gentle manual techniques, and lifestyle shifts that remove the constant triggers keeping the pelvic floor contracted.
Slow, diaphragmatic breathing with long exhales signals the nervous system to reduce tension in the pelvic floor and increases blood flow to the bulbospongiosus, which is essential for pain reduction. External perineal pressure, performed carefully at home or with guidance from a pelvic floor physical therapist, helps the muscle soften without forcing it.

